West Virginia patients are left in limbo over changing insurance coverage of obesity medications
Share:
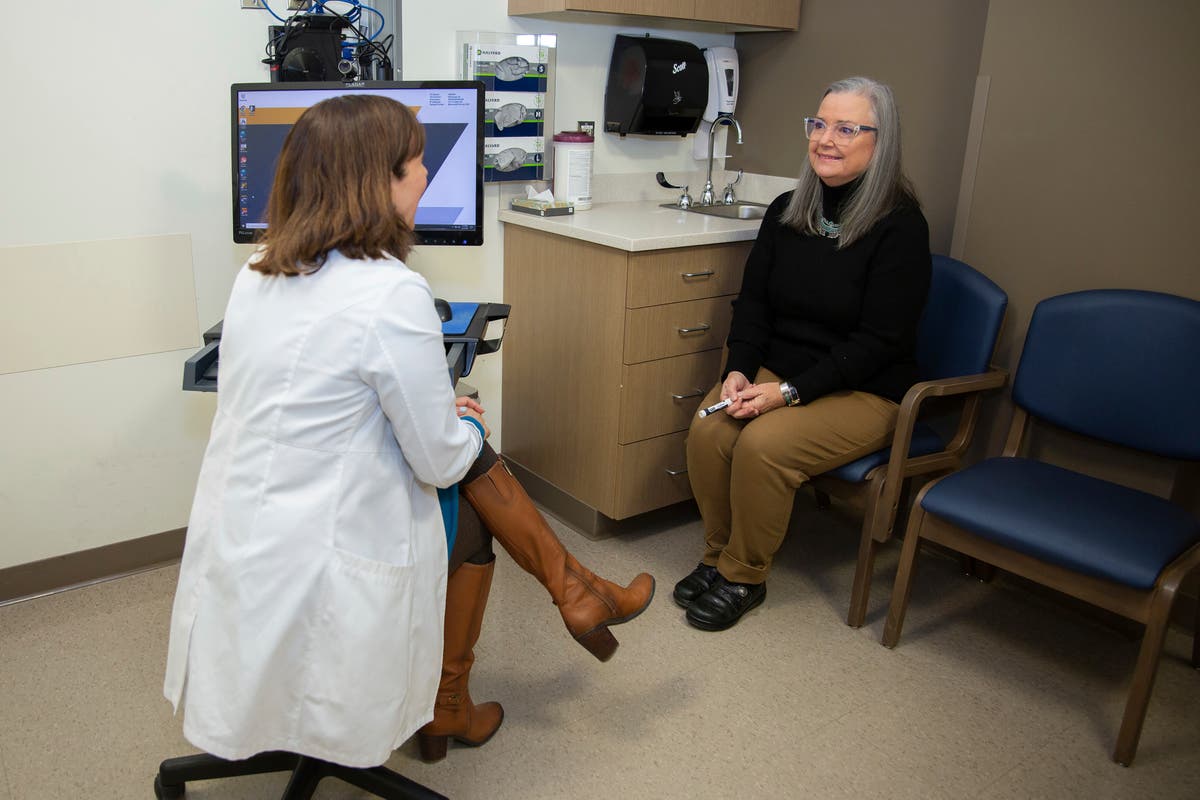
Lory Osborn says the Wegovy she was prescribed 15 months ago did more than help her lose 75 pounds — over a quarter of her body weight. The administrative assistant at West Virginia University said she feels healthier at 62 than she has since graduating high school.
But lately, she's been having panic attacks because she fears running out of medication. Citing a gross cost of $1.4 million a month, West Virginia abruptly announced in March it would indefinitely pause a pilot program covering weight loss drugs for 1,000 public employees, leaving patients like her scrambling. West Virginia’s Public Employee Insurance Agency (PEIA) will continue covering the popular and expensive GLP-1 drugs to treat Type 2 diabetes.
Other state and private insurers have adopted similar stances for the drugs, which can cost patients more than $1,000 monthly out-of-pocket. In 2024, Blue Cross Blue Shield of Michigan, the state’s largest nonprofit insurer, and North Carolina's state employee public insurance agency stopped covering the drugs for weight loss, saying the cost increased premiums for all customers.
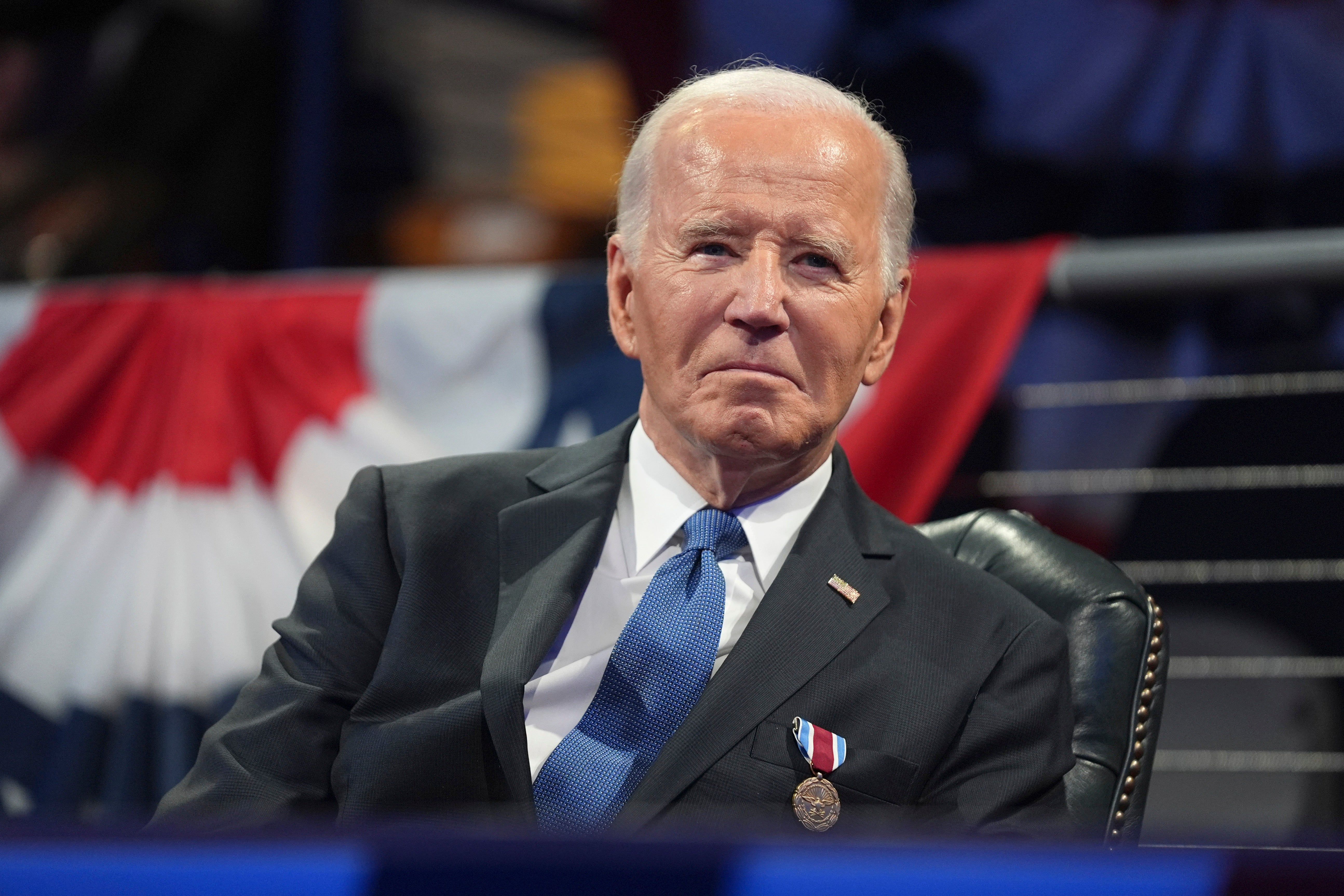
The dilemma comes amid a similar debate at the federal level. President Joe Biden unveiled a plan in November to cover the drugs for millions of weight loss patients on Medicaid and Medicare, though the measure could face opposition from President-elect Donald Trump's administration. Robert F. Kennedy Jr., Trump's nominee for Health and Human Services Secretary, has criticized Ozempic — a GLP-1 used to treat diabetes.